What are migraines?
If you’re a sufferer of migraines, you know there’s nothing else quite as debilitating. Often mistaken as an exaggerated headache, migraines are actually a neurological condition that are still very poorly understood. Migraine symptoms are felt body-wide and despite 1 in every 5 women and 1 in every 16 men being affected (1), the very first prescription migraine medication wasn’t approved by the FDA until 2018. Faced with a lack of medical understanding or accessible, effective treatments, people with migraines often shoulder the full weight of the condition in silence. Because of how overlooked they are, migraines are often misdiagnosed as headaches due to stress, dehydration or tension.
Migraine Symptoms
Headache or pain might be one of the most obvious symptoms of migraines; however, several different areas of the brain are activated during a migraine which can cause other symptoms such as:
- Sensitivity to light and sound
- Nausea and vomiting
- Pulsating or throbbing on one side of the head
- Poor concentration
- Feeling hot or cold

What are the different types of migraines?
Migraines Without Aura
Migraines without aura are the most common type of migraines. Essentially, there’s no warning sign that a migraine attack is coming on. The attack hits and can last anywhere from 4-72 hours. The pain and pulsating tends to localize to one side of the head and is accompanied by sensitivity to light and nausea. (2)
Migraines With Aura
Although auras actually take place in a different location in the brain, they have still been linked to migraines and are often referred to as a “warning sign” for the migraine attack. About 25 percent of migraine sufferers have an aura before the onset of other migraine symptoms. Auras are known to distort vision and cause blind spots. Aside from the visual disturbances, auras can also cause numbness, pins-and-needles, speech slurs and distorted sound. (3)
Episodic vs. chronic migraine
Episodic migraines are more sporadic, occurring 0 to 14 days of the month, whereas chronic migraines are classified as having headaches 15 days per month, with at least 8 of those days including other migraine symptoms. (4)
What causes migraines?
Magnesium Deficiency
Magnesium carries out a variety of crucial roles in the body like supporting nerve function, immunity and energy. One of its other main roles, the most important when discussing its link to migraines, is its ability to balance brain excitability by regulating glutamate (the main excitatory neurotransmitter) production. Why is this important? Migraines can be triggered by excessive neocortical cellular excitability and when magnesium levels are low, nerve cells release excess glutamate leading to brain excitability, and triggering a migraine.
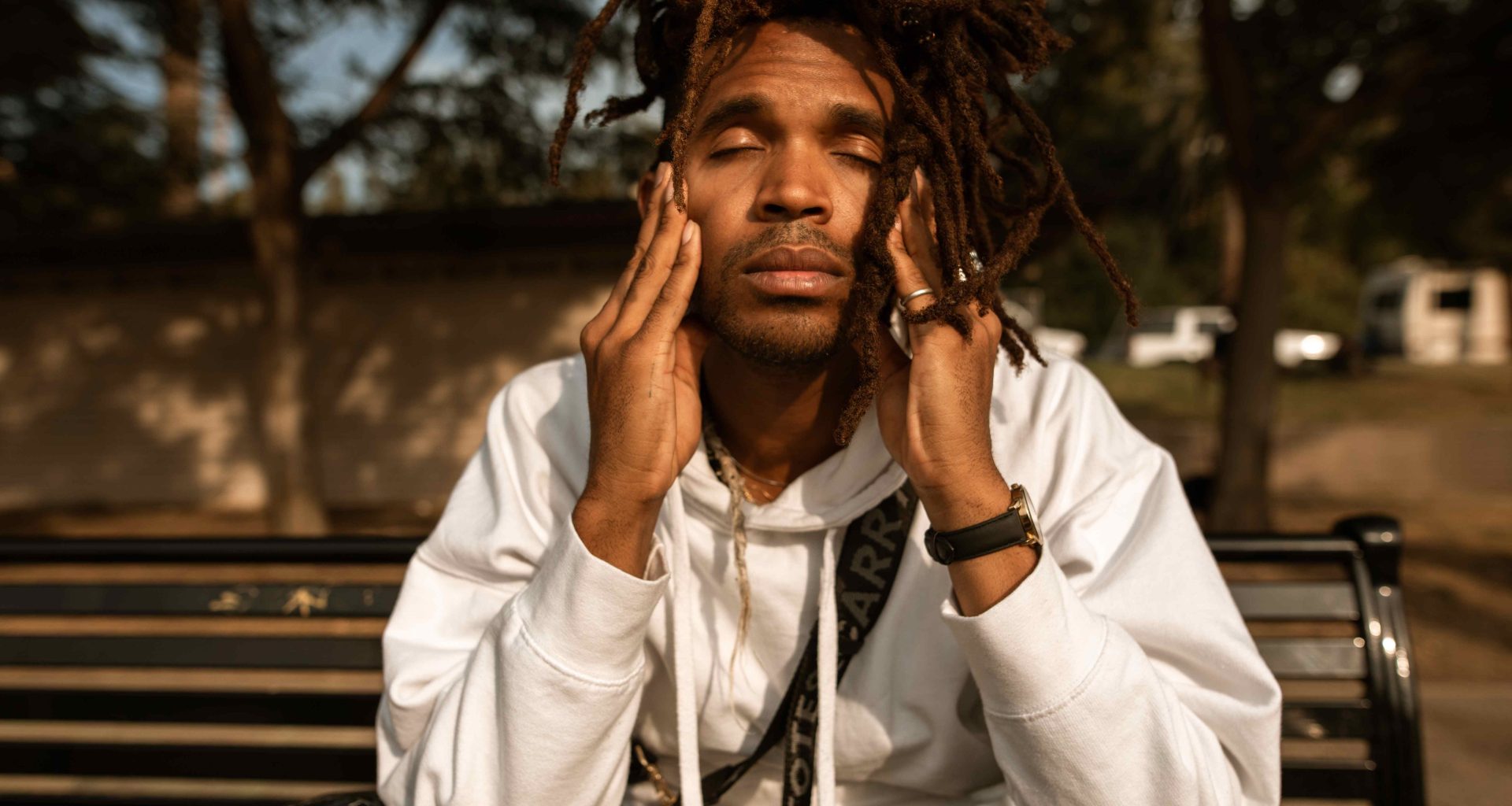
Stress
Did you know that 75-90% of all diseases are stress-related? Migraines are no exception with 70% of attacks being triggered by stress, (5) and most migraine patients report high levels of stress. To know if migraines are stress-induced, it’s important to pay attention to the body’s cues leading up to the attack. Fatigue, irritability, low appetite, upset stomach, muscle aches and weakness could all be signs that stress triggered the migraine.
Hormonal Imbalance
As mentioned, migraines tend to be more common in women and can be triggered during PMS, pregnancy and menopause due to the fluctuation in estrogen levels. Estrogen can also interfere with cellular excitability. There’s also a strong relationship between estrogen and neurotransmitters, and it’s been shown that estrogen can increase the release of glutamate. (6)
What is the trigeminal nerve?
The trigeminal nerve is one of the main nerves involved in migraines. In many cases, the generator area in the upper neck becomes overactive in people who experience migraines, causing a release of chemicals that trigger the expansion of blood vessels which can lead to symptoms associated with migraines. The trigeminal nerve branches into three more nerves in the face: a nerve that travels to the forehead, another that goes to the sinuses in the nose, and a third to the chin and jaw area. This can help explain why people tend to experience pain associated with migraine attacks in different locations.

How to Supplement for Migraines
Although prescription medication is available for migraines, they don’t always work for everyone, and can sometimes have unwanted side affects. Supplements and lifestyle changes can also help to reduce the severity and frequency of migraine attacks. Here are some of our top supplements for migraines.
Magnesium
Magnesium is one of the most recommended supplements for migraines. Magnesium deficiencies tend to be common among migraine sufferers and oftentimes it’s due to a genetic inability to properly absorb magnesium, so supplementation is key.
Beyond its ability to regulate glutamate, magnesium is involved in regulating blood flow and maintaining healthy blood vessels, which may be important in preventing the dilation and constriction of blood vessels that can trigger migraines. (7)
Magnesium also has a calming effect on the nervous system, which may help to reduce stress and anxiety, both of which can be triggers for migraines.
Keep reading for clinical evidence on the efficacy of magnesium for migraines below.
Riboflavin (Vitamin B2)
Riboflavin plays a crucial role in the energy metabolism of cells, including those in the brain. It is involved in the production of ATP, the main energy currency of cells, which can help to reduce mitochondrial dysfunction and oxidative stress, both of which are thought to contribute to migraines.
Riboflavin has also been shown to increase the production of glutathione, a potent antioxidant that can help to protect against oxidative stress and inflammation in the brain.
Riboflavin can help to enhance the function of the enzyme methylenetetrahydrofolate reductase (MTHFR), which is involved in the metabolism of homocysteine. (7) Elevated levels of homocysteine have been associated with an increased risk of migraines, and riboflavin supplementation has been shown to reduce homocysteine levels in migraine patients.
Read on for clinical evidence on the efficacy of riboflavin in the evidence section.
Feverfew
Feverfew is a plant that has been used for centuries to treat various ailments, including migraines. It is thought to reduce the production of prostaglandins, which are substances that can cause inflammation and pain in the body, and are believed to play a role in the development of migraines.
Feverfew is believed to inhibit the release of histamine, a chemical that is involved in the inflammatory response and can contribute to migraine symptoms.
Feverfew contains compounds called sesquiterpene lactones, which are thought to have anti-inflammatory and antioxidant properties. These compounds may help to reduce inflammation and oxidative stress in the brain, which are believed to be involved in the development of migraines. (8)
It is important to note that the quality and potency of feverfew supplements can vary widely, and some people may experience side effects such as mouth ulcers or digestive upset.
Coenzyme Q10
Coenzyme Q10 (CoQ10) is a naturally occurring substance that is involved in the production of ATP. It has been shown to be effective in reducing the frequency and severity of migraines, and is believed to work by several mechanisms.
CoQ10 has antioxidant properties, which can help to reduce oxidative stress and inflammation in the body—oxidative stress and inflammation have been linked to the development of migraines.
Mitochondrial dysfunction has been implicated in the development of migraines, and CoQ10 supplementation has been shown to improve mitochondrial function in people with migraines. (9)
CoQ10 has been shown to help regulate the production of neurotransmitters such as serotonin and dopamine, which are believed to play a role in the development of migraines.
Melatonin
Melatonin is a hormone produced naturally by the body’s pineal gland and is known to help regulate sleep-wake cycles.
Studies have shown that taking melatonin supplements for migraines can help reduce the frequency and severity in some people. In one study, people who took melatonin supplements daily for three months had a significant reduction in the number of migraines they experienced. (10)
Melatonin may also be helpful for people who experience migraines with aura—one study found that taking melatonin supplements before bed helped reduce the frequency and duration of migraine aura symptoms.

Lifestyle Remedies for Migraines
Physical therapy
Migraines are often associated with muscle tension in the head and neck region. Physical therapy can help to release this tension and improve overall muscle function by addressing underlying issues such as muscle tension, poor posture, and neck or jaw dysfunction.
Acupuncture
Acupuncture stimulates the release of endorphins, the body’s natural painkillers. It also helps to regulate the nervous system, including the part of the nervous system that controls pain. In one study, (11) researchers found that acupuncture was more effective than a placebo treatment in reducing the frequency and intensity of migraines. Another study (12) found that acupuncture was as effective as the medication propranolol in reducing the frequency of migraines. (13)
CBT/Biofeedback
Cognitive-behavioral therapy (CBT) is a form of psychotherapy that aims to change the negative thought patterns and behaviors that contribute to various physical and mental health conditions, including migraines. CBT for migraines typically involves teaching individuals skills to manage stress, identify and modify negative thought patterns, and adopt healthier lifestyle habits.
CBT can help by:
- Reducing stress: Stress is a common trigger for migraines, and CBT can help individuals learn to manage stress more effectively. This may include techniques such as relaxation training, mindfulness, and cognitive restructuring.
- Identifying and modifying negative thought patterns: Negative thought patterns can contribute to the development and maintenance of migraines. CBT can help individuals identify and challenge these patterns, and develop more positive and realistic ways of thinking.
- Developing healthy lifestyle habits: Certain lifestyle habits, such as poor sleep, irregular eating patterns, and lack of exercise, can trigger migraines. CBT can help individuals develop healthier habits that may reduce the frequency and severity of migraines.
A 2018 review (14) found that CBT was associated with significant reductions in migraine frequency and intensity.
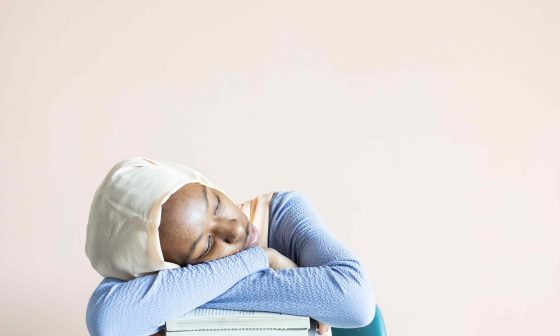
Meditation
Mindfulness-based interventions may help reduce the frequency and intensity of migraines, as well as improve quality of life for individuals living with migraines. (15) In addition to this, mindfulness can help with:
- Stress reduction: Stress is a common trigger for migraines, and mindfulness-based interventions can help individuals learn to manage stress more effectively.
- Pain management: Mindfulness-based interventions may also help individuals manage pain related to migraines. A 2022 study (16) found that mindfulness-based interventions were associated with significant reductions in pain intensity and frequency among individuals with chronic headaches.
- Emotion regulation: Migraines can be emotionally distressing, and mindfulness-based interventions may help individuals develop more effective ways of regulating their emotions.
Exercise
Regular exercise has been shown to reduce the frequency and severity of migraines, as well as improve overall physical and emotional well-being.
Exercise can help by:
- Improving cardiovascular health: Exercise can improve cardiovascular health, which may reduce the risk of developing migraines.
- Reducing stress: A 2018 study published in the Journal of Headache and Pain found that regular exercise was associated with significant reductions in stress and anxiety among individuals with migraines.
- Improving sleep: A 2017 study published in the Journal of Sleep Research (17) found that regular exercise was associated with significant improvements in sleep quality among individuals with migraines.
- Releasing endorphins: Exercise can also lead to the release of endorphins, natural painkillers, which can help reduce the intensity and duration of migraines.
Evidence
Dive deeper into the efficacy of two of our go-to supplements for migraines.
Magnesium
Magnesium is a vital mineral that plays a key role in various functions, including nerve and muscle function and neuromuscular excitability. Magnesium deficiency has been linked to cortical spreading depression, platelet aggregation, the release of substance P, neurotransmitter release and vasoconstriction. Magnesium deficiencies tend to be more common in migraine sufferers.
Studies:
- Research on magnesium has found that supplementation can be a well-tolerated, safe and inexpensive option to support migraines. In a study measuring ionized magnesium levels during a migraine attack, it was found that 50% had levels below 0.54 mmol/l (normal adult range 0.54-0.65 mmol/l) (18). With intravenous administration of 1g magnesium sulfate, 86% of patients who had low ionized magnesium levels reported sustained pain relief over 24 hours.
- A 2016 review of 21 studies (19) concluded that taking an oral magnesium supplement can help to prevent migraine attacks and reduce their frequency and intensity.
Riboflavin
The exact mechanism by which riboflavin prevents migraines is thought to be related to its role in energy production and antioxidant activity. Riboflavin is a cofactor for several enzymes involved in the production of energy in the body, including the electron transport chain in mitochondria. Riboflavin is also an important antioxidant, helping to protect cells from oxidative stress and damage. It has been suggested that riboflavin may prevent migraines by improving mitochondrial function and reducing oxidative stress in the brain.
Studies:
There have been several studies investigating the use of riboflavin for the prevention of migraines.
- A 2004 study published in the journal Headache (20) found that riboflavin supplementation (400 mg/day) was effective in reducing the frequency of migraines in a group of 41 patients. The study found that riboflavin was associated with a significant reduction in the number of migraines per month, as well as a reduction in the severity and duration of migraines.
- A 2015 meta-analysis published in the journal Headache found that riboflavin was effective in reducing the frequency and intensity of migraines in several randomized controlled trials. The meta-analysis included seven studies with a total of 549 patients and found that riboflavin was associated with a significant reduction in the number of migraines per month and a significant reduction in the intensity of migraines.
References
- Impact of migraine. The Migraine Trust. (2023, March 9). Retrieved March 23, 2023, from https://migrainetrust.org/understand-migraine/impact-of-migraine/
- Ruschel, M. A. P., & De Jesus, O. (2023, February 13). Migraine Headache. National Library of Medicine. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK560787/
- Kikkeri, N. S., & Nagalli, S. (2022, December 6). Migraine with Aura. National Library of Medicine. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK554611/
- Katsarava, Z., Buse, D. C., Manack, A. N., & Lipton, R. B. (2011, November 15). Defining the differences between episodic migraine and chronic migraine. Current pain and headache reports. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3258393/
- Maleki, N., Becerra, L., & Borsook, D. (2012, October). Migraine: Maladaptive brain responses to stress. Headache. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3475609/
- Del Río, J. P., Alliende, M. I., Molina, N., Serrano, F. G., Molina, S., & Vigil, P. (2018, April 27). Steroid hormones and their action in women’s brains: The importance of hormonal balance. Frontiers. Retrieved March 23, 2023, from https://www.frontiersin.org/articles/10.3389/fpubh.2018.00141/full
- Gaul, C., Diener, H.-C., & Danesch, U. (2015, April 3). Improvement of migraine symptoms with a proprietary supplement containing riboflavin, magnesium and Q10: A randomized, placebo-controlled, double-blind, multicenter trial. The journal of headache and pain. Retrieved March 23, 2023, from https://pubmed.ncbi.nlm.nih.gov/25916335/
- Pareek, A., Suthar, M., Rathore, G. S., & Bansal, V. (2011, January). Feverfew (tanacetum parthenium L.): A systematic review. Pharmacognosy reviews. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3210009/
- Sazali, S., Badrin, S., Norhayati, M. N., & Idris, N. S. (2021, January 5). Coenzyme Q10 supplementation for prophylaxis in adult patients with migraine-A meta-analysis. BMJ open. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7786797/
- Zduńska, A., Cegielska, J., & Domitrz, I. (2022, August 15). The pathogenetic role of melatonin in migraine and its theoretic implications for pharmacotherapy: A brief overview of the research. Nutrients. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9415653/
- Coeytaux, R. R., Kaufman, J. S., Kaptchuk, T. J., Chen, W., Miller, W. C., Callahan, L. F., & Mann, J. D. (2005, October). A randomized, controlled trial of acupuncture for Chronic Daily Headache. Headache. Retrieved March 23, 2023, from https://pubmed.ncbi.nlm.nih.gov/16178942/
- Allais, G., De Lorenzo, C., Quirico, P. E., Airola, G., Tolardo, G., Mana, O., & Benedetto, C. (2002, October). Acupuncture in the prophylactic treatment of migraine without aura: A comparison with flunarizine. Headache. Retrieved March 23, 2023, from https://pubmed.ncbi.nlm.nih.gov/12390610/
- Linde, K., Allais, G., Brinkhaus, B., Fei, Y., Mehring, M., Vertosick, E. A., Vickers, A., & White, A. R. (2016, June 28). Acupuncture for the prevention of Episodic Migraine. The Cochrane database of systematic reviews. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4977344/
- Bae, J. Y., Sung, H. K., Kwon, N. Y., Go, H. Y., Kim, T. J., Shin, S. M., & Lee, S. (2021, December 28). Cognitive behavioral therapy for Migraine Headache: A systematic review and meta-analysis. Medicina (Kaunas, Lithuania). Retrieved March 23, 2023, from https://pubmed.ncbi.nlm.nih.gov/35056352/
- Wells, R. E., Beuthin, J., & Granetzke, L. (2019, February 21). Complementary and integrative medicine for episodic migraine: An update of evidence from the last 3 years. Current pain and headache reports. Retrieved March 23, 2023, from https://pubmed.ncbi.nlm.nih.gov/30790138/
- Wells, R. E., Seng, E. K., Edwards, R. R., Victorson, D. E., Pierce, C. R., Rosenberg, L., Napadow, V., & Schuman-Olivier, Z. (2020, March). Mindfulness in migraine: A narrative review. Expert review of neurotherapeutics. Retrieved March 23, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7213534/
- Knufinke, M., Nieuwenhuys, A., Geurts, S. A. E., Coenen, A. M. L., & Kompier, M. A. J. (2017, March 8). Self-reported sleep quantity, quality and sleep hygiene in elite athletes. Journal of Sleep Research. Retrieved March 23, 2023, from https://onlinelibrary.wiley.com/doi/full/10.1111/jsr.12509
- Nechifor, M., & Vink, R. (2011). Magnesium in the central nervous system. University of Adelaide Press.
- Chiu, H. Y., Yeh, T. H., Huang, Y. C., & Chen, P. Y. (2016, January). Effects of intravenous and oral magnesium on reducing migraine: A meta-analysis of randomized controlled trials. Pain physician. Retrieved March 23, 2023, from https://pubmed.ncbi.nlm.nih.gov/26752497/
- Blau JM;, J. N., Kell, C. A., & Sperling, J. M. (2004, January). Water-deprivation headache: A new headache with two variants. Headache. Retrieved March 23, 2023, from https://pubmed.ncbi.nlm.nih.gov/14979888/